Psychosis among drug users is quite common. Often, it is difficult to determine which came first, substance use or psychosis. Frequently, they co-occur. In cases where drugs are causally related (i.e.,
substance-induced psychosis), the condition is typically transient with a duration of 1 month or less. In rare cases, the length of psychosis can last longer. And in even rarer cases, symptoms such as hallucinations can be permanent.
Psychosis can be associated with the use many legal (e.g.,
alcohol) or illicit substance such as stimulants (
amphetamines and
cocaine),
cannabis, and
hallucinogens. An article by Thirthalli and Benegal (
1) reviews the evidence that these drugs can cause psychosis in nonpsychotic persons.
Alcohol
The neurochemical effects of alcohol are complex. "Common knowledge" states that alcohol acts in a similar fashion to other sedatives (e.g., diazepam). In other words, it is an
agonist of
GABA receptors. In reality, the alcohol molecule is very simple. It has the ability to cross cell membranes (e.g.,
blood-brain barrier) easily and can exert its effects on the brain within minutes. Alcohol also influences the
phospholipid bilayer that make up
cell membranes. This ability has a widespread impact on normal cell functions and also enables alcohol to modify the action of many
neurotransmitter systems, such
glutamate,
dopamine, and
norepinephrine in addition to GABA.
Alcohol-induced psychosis can occur during different drug states such intoxication or withdrawal (e.g.,
delirium tremens,
alcoholic hallucinosis). In general, the risk of psychosis is two-fold greater than in the general adult population.
Stimulants (click to enlarge picture;
2)
Cocaine and Amphetamines are widely known to lead to psychosis. The psychosis produced by both cocaine and amphetamines is similar to schizophrenia. The risk of psychosis from amphetamine use is quite high; greater than 70% in chronic users. Users who develop first episode psychosis use an average of 20 times years. Psychosis typically lasts for the duration the drug is in the system. However, it can last more than a month in more severe cases.
For cocaine, typically 50% of chronic users experience paranoia and hallucinations. Cocaine-induced psychosis has a stereotypical form; Users believe that their drug use is being watched and that they are being followed. This paranoia is typically accompanied by hallucinations. Cocaine-induced psychosis also shows sensitization; that is, psychosis becomes more severe and occurs more rapidly with continued use. Unlike amphetamine-induced psychosis, cocaine induced-persistent psychosis is very rare.
Cocaine has the highest affinity and binds most strongly to the
serotonin (5HT)reuptake pump, followed by the dopamine (DA) reuptake pump, then the norepinephrine (NE) reuptake pump (FYI-Effexor is cocaine with a PG-rating; effexor's affinities are for serotonin, then NE, and then DA). Contrary to popular belief, amphetamines do not act by blocking the dopamine reuptake pump. Amphetamines are
indirect agnonist of the
catecholaminergic systems (i.e., dopamine and norepinephrine). First, amphetamines go inside the neuron and release both DA and NE from their vesicles into the cell cytoplasm (i.e., catecholamins are released inside the neurone). Second, The catecholamines are subsequently transported outside of the neuron by a reversal of the reuptake pumps. This results in a MASSIVE increase in synaptic DA and NE. Lastly, at higher doses, amphetamines inhibit catecholamine metabolism, leading to even higher concentrations in the synapse.
Cannabis
There has been a boom in the current research of cannabis and psychosis. There appears to be a temporal correlation between early cannabis use and onset of schizophrenia. This association is stronger than for any other substance. Why the association exists is unclear. In general, cannabis has the same risk of inducing psychosis as alcohol (i.e., two-fold).
There are two cannabinoid receptors in the human body:
CB1 and
CB2. The CB2 receptor is not expressed in the brain, and is primarily found in the immune system. The CB1 receptor is typically found in the basal ganglia, cerebellum, hippocampus, and the cortex. CB1 receptors exist on the
axon terminal instead of the
post-synaptic cell. In others words, CB1 receptors are
autoreceptors that can inhibit the release of many different neurotransmitters.
Hallucinogens
Many different drugs fall under this category: mushrooms,
peyote buttons, and
LSD, for example. Many hallucinogenic drugs are either synthesized by plants or are based on plant-derived compounds. The main active compound in peyote is
mescaline, while
psilocin in found mushrooms. LSD is actually a synthetic compound, but is based on a fungal alkaloid taken from
ergot.
Hallucinogenic compounds have a catecholamine-like structure (most are similar in shape to serotonin). Hallucinogens are primarily 5-HT2a receptor agonists. While these drugs do not lead to dependence, withdrawal, or cravings, they still can lead to serious problems for some users. Some people experience acute anxiety or panic attacks in responses to the drugs' hallucinogenic effects. There is a disorder known as hallucinogen persisting perception disorder (HPPD), which is the fancy name for "flashbacks." The most severe reactions, of course, are psychotic breakdowns. However, similar to the above mentioned drugs, psychosis is typically transient. Most prolonged episodes of hallucinogen-induced psychosis involve individuals who have already been diagnosed with a psychotic disorder or who have manifested prepsychotic (e.g., prodromal) symptoms before taking these drugs.
Treatment
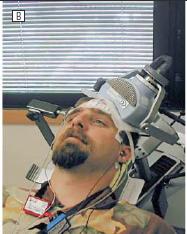
In most cases, substance induced psychosis does not need medical treatment per se. It usually disappears when the drug's affects are gone. However, there are cases when treatment is necessary. Alcohol dependent individuals in withdrawal do need medical treatment because
alcohol withdrawal can be lethal. Typically, sedatives (
benzodiazepines) are the drugs of choice. For either cocaine or amphetamine induced psychosis,
first or
second generation antipsychotics are the drugs of choice because of their potent
D2 receptor antagonism. In general, it is common for anyone presenting with psychotic symptoms to be prescribed antipsychotics. Occasionally, patients who are addicted to amphetamines will be prescribed antipsychotics in hopes that they will reduce the risk of subsequent psychosis or reduce euphoria, making the drug less reinforcing. Drugs that antagonize the 5HT2a receptor such as
risperidone (or any second generation antipsychotic),
ketanserin, and
ritanserin have been shown to reverse hallucinogenic-induced psychosis.
In rare cases when psychosis persists, there are a few things to consider, such as, is their another cause for the psychosis? For example, does the person have schizophrenia or is there a physical cause for the psychosis (e.g., tumor, metabolic, etc)? Often times, doctors not knowing what to do, will double down on the antipsychotics. This is unlikely to work because the mechanism of action (D2 or 5HT2a blockade) does not necessarily increase with the addition of a second drug. Simply upping the does of the current drug should suffice. Side effects, however, are always additive. Antipsychotics with higher affinities for both D2 and 5HT2a receptors are preferable (e.g., risperidone).
Risk Factors
The risk factors for substance-induced psychosis are similar across all substances. Pre-morbid psychiatric history or a family history of schizophrenia put an individual at risk. Also, the longer a substance is consumed and the larger the quantities consumed are also risk factors. Polysubstance use or consuming drugs that contain other compounds increases the risk of psychosis too. Unfortunately, the research into the neurobiological and genetic underpinnings is substance-related psychosis are quite poor. A useful theory for substance-related psychosis which could lead to better acute treatment is lacking.
 Thirthalli, J & Benegal, V. (2006). Psychosis Among Substance Users Current Opinion in Psychiatry
Thirthalli, J & Benegal, V. (2006). Psychosis Among Substance Users Current Opinion in Psychiatry